Research Article
Abstract
Sport psychologists are increasingly confronted with performance problems in sport where athletes suddenly lose the ability to execute automatic movements (Rotheram, Maynard, Thomas, Bawden, & Francis, 2012). Described as performance blocks (Bennett, Hays, Lindsay, Olusoga, & Maynard, 2015), these problems manifest as locked, stuck, and frozen movements and are underpinned by an aggressive anxiety component. This research used both qualitative and quantitative methods in a single case study design to investigate the effectiveness of eye movement desensitization and reprocessing (EMDR) therapy with graded exposure as a treatment method. The participant was a 58-year-old professional male golfer who had been suffering a performance block for 11 years. Specifically, the participant was experiencing involuntary spasms, shaking, muscle tension, and jerking in the lower left forearm while executing a putting stroke. Physical symptoms were coupled with extreme anxiety, panic, and frustration. The study tested the hypothesis that reprocessing related significant life events and attending to dysfunctional emotional symptoms would eliminate the performance block and related symptoms and that the individual would regain his ability to execute the affected skill. Pre-, mid-, and postintervention performance success, using the Impact of Event scale, subjective units of distress (SUD; Wolpe, 1973), and kinematic testing revealed improvements in all associated symptoms in training and competition. These findings suggest that previous life experiences might be associated with the onset of performance blocks and that EMDR with graded exposure might offer an effective treatment method.
A performance block is a phenomenon in sport in which physical movement is momentarily disrupted, causing an inability to perform skills that were once effortless (Bennett et al., 2015). Traditionally, performance blocks have been considered under disparate labels, for example, the yips in sports such as golf and cricket and lost move syndrome (LMS) in gymnastics, trampolining, and diving (Day, Thatcher, Greenless, & Woods, 2006; Rotheram, Thomas, Bawden, & Maynard, 2007). There is evidence to suggest that the root causes of these problems are psychological in nature and that they might, in fact, be forms of the same disorder (e.g., Bennett et al., 2015; Bennett et al., 2016; Roberts, Rotheram, Maynard, Thomas, & Woodman, 2013). Indeed, recent research exploring these entities collectively has reported numerous psychological similarities between them, including intense cognitive anxiety, loss of control, fear, intrusive thoughts, and frustration, the primary factor being an extreme level of anxiety during and following initial onset of the problem (Bennett et al., 2015). Thus, it was proposed that the yips and LMS be reconsidered as one and the same form of disorder (Bennett et al., 2015). The generic term performance block was put forward, described as severe cognitive and somatic anxiety, muscle spasms, locked, stuck, and/or frozen movement, and a momentary loss of cognitive and motor control (Bennett et al., 2015).
Performance Blocks and Anxiety-Related Disorders
Similarities have been drawn between performance blocks in sport, anxiety-related disorders, and dystonia (cf. Rotheram et al., 2007). For example, typical symptoms associated with dystonia include sudden and uncontrolled movement disruption, extreme anxiety, fear, intrusive thought patterns, loss of control, and panic (Altenmüller, Ioannou, & Lee, 2015). Similarly, anxiety-based disorders involve components such as extreme cognitive and somatic anxiety, intrusive thoughts, obsessive behavior, loss of control, and fear (American Psychiatric Society [APA], 2013), all of which are major components of performance blocks (Bennett et al., 2015). Dystonic problems have been explained using dissociation theories and the conversion of psychological pain into physical symptoms (i.e., spasms, jerks, and freezing) as a form of defense against the painful emotional effects of remembering a traumatic event (Thomas, Vuong, & Janovic, 2006). It is suggested that the overwhelming intensity of emotion experienced during trauma floods the brain’s capacity to effectively process the event. Thus, rather than being stored appropriately in memory networks, an imprint of the experience is stored in its raw emotional and sensory form (Scaer, 2014). In accordance with dissociation theory, environmental stimuli vaguely connected to a past traumatic experience (including emotion, image, sensation, cognition, belief, or environmental) can cause the same emotional and sensory components attached to the past event to resurface (LeDoux, 2014; Levine, 1997).
The Impact of Significant Life Events
There is increasing evidence demonstrating a link between unprocessed memories and psychological disorders (Logie, 2014), and it has previously been suggested that psychologically significant life events experienced away from the sporting context might be a factor in the onset of the yips (Roberts et al., 2013; Rotheram et al., 2007). In their study exploring the yips in golf, Rotheram et al. (2007) demonstrated a link between the yips and a history of significant life events (e.g., death of a loved one, relationship breakdown). In another study, Bawden and Maynard (2001) found that psychologically significant sport-related events (e.g., dropped catch, embarrassment, arguments) occurred immediately prior to the first yips experience in cricket bowlers. Day et al. (2006) also suggested that LMS was equivalent to a traumatic experience and might therefore trigger comparable behavioral responses to those of trauma victims. Taken together, existing literature suggests that psychological characteristics associated with the lived experience of performance blocks (e.g., loss of cognitive control, intense fear, panic, anxiety), as well as reported coping mechanisms (e.g., avoidance behavior, dissociation), might involve subconscious processes and be linked to a history of significant life events that have been stored as unprocessed imprints in the brain. Thus, it is perhaps unsurprising that researchers and applied practitioners have faced major difficulties in identifying a successful treatment method for performance blocks (Klämpfl, Lobinger, & Raab, 2013; Rotheram et al., 2007).
Lack of an Effective Treatment Method
Treatment for performance blocks has largely composed of cognitive behavioral techniques and/or technical modifications to the affected skills such as visualization, self-talk, changing hand grip on the golf club, eliminating a specific rotation from a dive (Philippen, Legler, Land, Schuetz, & Schack, 2014). If performance blocks are indeed psychologically centered, somewhat subconscious, and associated with significant life events, it is essential to explore treatment methods that purposefully target these factors. Early treatment methods for anxiety-based disorders and trauma victims have primarily revolved around talking therapies and drug prescription (Ho & Lee, 2012; Shapiro, 2001). Considering the growing body of research implying that memories associated with traumatic experiences are associated with anxiety-based problems and psychological disorders (Scaer, 2014), it is not surprising that increased interest is being directed toward therapies that facilitate the identification and reprocessing of traumatic memories (e.g., emotional freedom technique [EFT]; Craig, 1999, and eye movement desensitization and reprocessing [EMDR]; Shapiro, 2001). To date, only one published study has attempted to use EFT in sport. In their study, Rotheram et al. (2012) applied EFT to a yips-affected golfer. Following four sessions of EFT to address the cognitive and emotional symptoms of the yips, the authors reported symptom relief and improved putting performance. Although this research adds valuable evidence toward the potential success of these therapies, the scientific evidence base for EFT is very much in its infancy and much further research is required.
EMDR as an Effective Treatment Method
Since its initial application as a treatment therapy for posttraumatic stress disorder (PTSD; e.g., Novo Navarro et al., 2016), EMDR therapy has been successfully used to treat various disorders including generalized anxiety disorder (Gauvreau & Bouchard, 2008), depression (Grey, 2011), fear and posttraumatic anxiety (Dautovic, de Roos, van Rood, Dommerholt, & Rodenburg, 2016), and obsessive-compulsive disorder (Marr, 2012). EMDR has also been formerly recognized as the treatment of choice for PTSD-related disorders by a wide range of clinical organizations including the APA (2013), the National Institute for Health and Care Excellence (NICE; 2005), and the World Health Organization (2013). The integrative eight-phase treatment design is based on the adaptive information-processing model (AIP; Shapiro, 2001, 2007). This model suggests that memories attached to traumatic experiences are not adequately processed but instead stored in real time, as emotional and somatic symptoms. If left unprocessed, the emotional and somatic symptoms attached to the original event will continue to resurface as if in the present, causing extreme hyperarousal, anxiety, and avoidance of stimuli even vaguely connected to the original memory. Through directed dual attention (recalling the memory while remaining grounded in the present, assisted by bilateral stimulation), the brain can access the dysfunctionally stored memories, stimulate the brains natural processing system, and bring the memory to an adaptive resolution. Once the memory has been fully processed, the necessary information is assimilated and new information can be appropriately stored in memory without the disturbing emotional and physical sensations that were originally attached. Unlike traditional cognitive therapies that deliberately challenge, restructure, and then reframe negative beliefs into adaptive rational ones, EMDR therapy facilitates the spontaneous shifting of the negative belief during subsequent processing (Oren & Solomon, 2012). EMDR therapy requires the client to focus on the traumatic memory for only a short time, gaining a sense of mastery through the ability to move between the present and the past event during each set of bilateral stimulation.
EMDR Therapy for the Treatment of Performance Anxieties
The predominant components of performance blocks appear to be cognitive and somatic anxiety and impaired performance. It is therefore appropriate to briefly discuss literature investigating the use of EMDR therapy specifically for the treatment of anxiety-related performance problems. Several studies have applied EMDR to performance anxiety with relatively consistent findings. For example, Cook-Vienot and Taylor (2012) delivered the standard EMDR protocol to 30 participants suffering test anxiety in an attempt to compare its effectiveness with biofeedback and stress inoculation training (SIT). After an initial 45-minute introduction and a further three 75-minute sessions, the authors reported significantly lower posttreatment scores on the test anxiety scale for EMDR and also improved levels of state and trait anxiety, although these were not significantly different to biofeedback/SIT. Maxfield and Melnyk (2000) also found a single session of EMDR significantly reduced test anxiety symptoms in 17 test anxious students who received treatment either immediately or after posttest measures (the latter group were informed they were on a waiting list). Specifically, both immediate and delayed EMDR generated improved scores on the test anxiety inventory and the fear of negative evaluation scale (Maxfield & Melnyk, 2000).
In another study, Barker and Barker (2007) used an adapted EMDR protocol originally developed by Lendl and Foster (1997) for performance enhancement (cf. Lendl & Foster, 1997). In their study, Barker and Barker (2007) treated a single case of presentation anxiety (anxiety associated with communicating in front of a large audience) to test the hypothesis that presentation anxiety was caused by previous trauma experience and associated negative beliefs and that EMDR would allow for trauma memories to be effectively processed and positive cognitions installed. In a 12-month follow-up, authors reported reduced anxiety associated with the problem and alleviated anxiety symptoms (reduced heart rate, sweating, nausea, and panic). They concluded that the adapted EMDR protocol effectively reduced presentation anxiety. Using the same protocol, Ricci and colleagues (2009) suggested EMDR alleviated physiological (elevated heart rate, sweating, nausea), cognitive (loss of focus and concentration), emotional (fear and panic), and behavioral (avoidance) symptoms associated with performance anxiety.
Considering the underpinning components of performance blocks (i.e., anxiety, fear, intrusive thoughts, loss of control), it stands to reason that a therapeutic intervention that has proven so effective in treating disorders underpinned by anxiety, and those related to trauma, would be equally promising for performance blocks.
Trauma-Focused Cognitive-Behavioral Therapy
A common feature of treatment protocols for anxiety problems is trauma-focused CBT (NICE, 2005). This method is based on the premise that individuals who have symptoms of an acute anxiety disorder as a result of a traumatic experience also have unhelpful thoughts and beliefs specifically related to the event. Consequences of these thoughts and beliefs include avoidance behavior and hypervigilance to perceived threatening events that might remind the person of the threatening situation (either cued or uncued). A major component of trauma-focused CBT is graded exposure that aims to reduce avoidance through repeated exposure to the threatening cue, while challenging unhelpful/harmful thoughts/beliefs associated with the stimuli (Craske, Treanor, Conway, Zbozinek, & Vervliet, 2014). In essence, exposure treatment works on the premise that repeated reexposure to anxiety-inducing stimuli effectively reduces a learned fear response by creating a new, more appropriate response (Kindt, 2014). The context in which performance blocks are experienced requires a direct need for the individual to reenter the problem-associated environment to train and compete. Thus, gradual supported exposure might provide an effective framework through which this process can occur.
Aims of the Current Study
The primary aim of this study was to explore the effectiveness of a combined intervention of EMDR therapy and graded exposure for the treatment of performance blocks. Because of the lack of existing research using EMDR for performance block type problems in sport, a second aim was to comprehend the individual’s experience of receiving EMDR within the context of elite sport and to ascertain any sport-specific considerations that might need to be addressed. It is hypothesized that reprocessing significant life events and attending to dysfunctional emotional symptoms will eliminate the performance block and related symptoms and that the individual will regain their ability to execute the affected skill.
Method
Participant
Following institutional ethics approval, qualitative and quantitative methods were adopted to assess the effectiveness of EMDR therapy with exposure therapy to treat a professional golfer who had been suffering a performance block for 11 years, consequently disabling him from executing the putting stroke. The participant (X1) was identified to the primary researcher by a professional coach at his club who was aware of the research being conducted following previous involvement in other studies. X was a 58-year-old, White British male golfer who presented with all of the criteria for a type of performance block commonly referred to as the yips (Rotheram et al., 2007). Specifically, X was experiencing involuntary spasms, shaking, muscle tension, and jerking in the lower left forearm while executing a putting stroke both in practice and competition. Physical symptoms were coupled with extreme anxiety, panic, and frustration. When asked to describe his first experience of this problem, he stated,
There was a sensation of a muscle spasm in my left wrist, a vibration and tightness which I couldn’t control; there was nothing I could do about it. It was like a brake and accelerator fighting each other I’ve no idea where it came from; it just suddenly appeared. It’s like a mental illness now; it’s fearful and I don’t know when it’s going to happen.
The problem first occurred in competition 11 years prior to this study, when the participant was attempting a 3-foot putt on the 18th green. For a few weeks after this, he experienced no further disturbance; however, the problem later returned during a noncompetitive game. X recalled how the problem suddenly returned and quickly escalated: “It came back absolutely out of nowhere and then built up and up and up, to the point it got worse and worse, and bigger and bigger, and you can’t control it; you just can’t play anymore.” After 30 years competing at major championship events, and 8 more years struggling with a performance block, X was ultimately forced to retire 3 years prior to this study.
X reported several attempts at overcoming the problem using different technical adjustments (e.g., using a long putter, putting with one hand, standing at a different angle, and using a weighted club), none of which had alleviated symptoms: “I’ve changed stances, used longer putters, shorter putters, heavier putters, all these sorts of things but it’s not worked remotely; I can still feel it.” X also described extreme and persistent anxiety, nervous dread related to golf, disturbed sleep, avoidance of the environment and associated conversation, ruminative thought patterns, fear of the skill, damaged relationships, and isolation. Finally, when asked if he was able to visualize himself successfully putting, he stated, “I can’t even see the positive image anymore.”
EMDR Therapist
The therapist involved in the delivery of EMDR was a consultant clinical psychologist registered with the Health Care Professions Council (HCPC) and certified in EMDR. He has over 15 years of experience providing mental health care and training to a range of organizations. He also has experience providing mental health care in the context of elite sport. On initial contact with the therapist, the primary researcher described the case and discussed the extent of his involvement should he wish to proceed. The therapist confirmed his interest, and as there was no existing relationship between the therapist and participant, an initial meeting was arranged.
Sport Psychologist
The sport psychologist was a chartered member of the British Psychological Society and registered with the HCPC. He has over 15 years of experience working in elite sport with various high-performance teams. He was known to the primary researcher prior to the start of this study and on discussing the case immediately expressed interest in supporting the intervention, specifically with the delivery of the exposure treatment element.
Pre- and Postintervention Performance Measures and Intervention Assessment
Treatment progress was assessed using a range of qualitative and quantitative methods pre-, during-, and posttreatment.
Prevalence of Performance Block Symptoms
Consistent with previous research (e.g., Marquardt, 2009; Rotheram et al., 2012), pre- and postintervention prevalence of the yips was assessed using visual inspection (where 0 = no yips and 1 = yips) and kinematic data. Specifically, before and after the intervention, the participant was required to perform 10 putts on a level putting green to each of 2 target holes at 0.91 m (3 ft) and 1.22 m (4 ft) distances. Distances were identified according to the participant’s most anxiety-inducing situation associated with the yips. Conditions were mild, dry, and with a light breeze on both occasions. To assess the degree and nature of movement disturbance in the forearms, three-dimensional kinematic data were captured using an electromagnetic sensor positioned 2.5 cm below the base of the putter grip (Polhemus Liberty, Polhemus Inc, Colchester, VT). Data were sampled at 240 Hz and captured using Golf Biodynamics Ultimate System software (Version 11.0.5, GBD Pty, Australia). As per manufacturer’s instructions, an electromagnetic pointer was used to digitize virtual markers used to define the target line. A local coordinate system for the putter was aligned such that the x-axis was coincident with the target line (positive direction away from the hole); y-axis was perpendicular to the target line (positive direction anterior to the participant); z-axis was vertically upward. The key kinematic variables derived from biomechanical analysis included putter face rotation angle and putter face rotation angular velocity. These data were exported using customized MATLAB script (The Mathworks Inc, Natick) and graphed in Microsoft Excel software.
Subjective Units of Distress (SUD; Wolpe, 1982)
SUD scores were recorded throughout EMDR and exposure treatment processes. This was to identify the participant’s subjective level of anxiety (where SUD 0 = no anxiety experienced and SUD 10 = extreme anxiety). These scores also provided a means of monitoring the success of each EMDR session where the aim was to reduce all SUD scores to less than 3 (Shapiro, 1999).
Validity of Cognition Scale (VOC; Shapiro, 2001)
VOC scores were recorded throughout EMDR treatment to monitor the level of belief the participant held in the positive cognitions associated with the problem (where VOC 1 = cognition is totally false and VOC 7 = cognition is totally true).
Impact of Event Scale (IES; Zilberg, Weiss, & Horowitz, 1982)
Consistent with previous research (e.g., Bennett et al., 2016), the IES was adopted as an additional measure of anxiety response to the EMDR treatment. Specifically, this measure assesses trauma-related symptom responses within the subscales: intrusion (intrusively experienced ideas, images, feelings, and/or dreams), avoidance (conscious avoidance of ideas, feelings, or situations related to the event), and physiological arousal (experience of anxiety-related symptoms manifesting in the body: cf. Sundin & Horowitz, 2002). The participant completed the measure pre- and postintervention, responding to each statement to indicate the level of distress experienced in relation to the problem. Distress level was reported using a scale of 0 (not at all) to 4 (extremely), with a total range of 0–88. Intrusive responses were measured by items such as “I thought about it when I didn’t mean to,” avoidance was measured by items such as, “I stayed away from reminders about it,” and physiological arousal was measured by items such as “My feelings about it were kind of numb.” It is recommended that total scores greater than 19 are high and that total scores between 30 and 60 are typical of PTSD sufferers (Zilberg et al., 1982).
Social Validation
Postintervention interviews were conducted with the participant, sport psychologist, and EMDR therapist to assess effects of the intervention and any behavioral changes that coincided with improved performance and symptom reduction. The interview schedule was constructed using a deductive approach to create a predetermined set of themes and categories (Patton, 2002). Interview questions were designed to provide the following: information relating to the participant’s experience of EMDR and its overall effectiveness for the treatment of performance blocks (e.g., extent of symptom reduction), information from the EMDR therapist outlining the procedure followed, and information from both practitioners regarding overall effectiveness of the intervention. This process was supported by the collection of session-by-session data. Interviews were conducted in the participant’s natural performance environment on completion of treatment. Following data collection, the primary researcher transcribed all interviews verbatim. No formal content analysis was performed on the transcripts; however, the full research team studied each transcript highlighting and discussing common themes relating to the treatment protocol and treatment effects. Where appropriate, extracts from the raw data have been directly included in the results.
Intervention
The intervention consisted of EMDR therapy combined with exposure therapy to treat a performance block. Prior to the start of the intervention, the sport psychologist and EMDR therapist met with the participant and familiarized themselves with the environment, establishing rapport with X through general discussion about golf. The total intervention period covered 27 weeks from inception to the final review session conducted 5 weeks posttreatment. During this period, five formal sessions were conducted between the EMDR therapist and X, regular exposure therapy with the sport psychologist, as well as independent practice supported by informal communication with the sport psychologist, and continued communication between the sport psychologist, EMDR therapist, and participant throughout the process. Issues regarding confidentiality were discussed during the first meeting, and X provided informed consent to continue. It was made clear that withdrawal from the study was permitted at any time up until the point of publication. Detail pertaining to formal contact sessions is provided in the following, with the exception of informal weekly updates.
EMDR Protocol
Consistent with previous research in studies where fidelity of treatment using EMDR therapy in case studies was high (e.g., Lipke & Botkin, 1993; Russel, 2006), the eight-phase standard EMDR protocol was adopted (Shapiro, 2001). Specifically, two sessions focused on Phases 1 and 2: client evaluation (including full mental health assessment and completion of the IES), case formulation, history taking, and client preparation. Additional focus was placed on educating X on EMDR, performance blocks, and anxiety. Reprocessing of target memories (TM’s) was covered in two separate sessions, each lasting approximately 120 minutes. A final review session took place 5 weeks posttreatment (including postintervention IES completion). To monitor the integration of exposure treatment with EMDR and to ensure that both practitioners were kept fully informed on treatment as it progressed, the EMDR therapist and sport psychologist were in communication before and after all sessions.
Graded Exposure
Exposure therapy was delivered by the sport psychologist and involved weekly sessions of in vivo exposure to harmless but distressing, problem-related stimuli. These sessions were delivered at the participants training venue and were all carried out separately to EMDR. Exercises were hierarchically arranged from least to most anxiety-evoking, as identified by X (Table 1). Specifically, X was guided through the process of identifying a series of situations associated with the performance block, toward which he experienced increasing levels of anxiety (where SUD 0 = no anxiety experienced; SUD 10 = extreme anxiety). These boundaries were more specifically defined by X (as SUD 0 = feeling the speed of my arms, control of my arms, and inner calmness and SUD 10 = electric shock in my arms, not in control of my arms, intense anxiety inside). X identified seven levels, with lowest anxiety associated with putting on the green alone (SUD = 2/10) and highest anxiety associated with playing an individual event with a scorecard (SUD = 10/10). Once each level was identified, the importance of weekly practice sessions was discussed, during which X would target each level progressively, recording relative SUD scores.
| Step | SUD Score (0–10) |
|---|---|
| Playing an individual event and entering a scorecard | 10 |
| Playing a round as part of a team | 9 |
| Game scenario with two other players | 8 |
| Putting with another pro on the green | 7 |
| Putting with another player on the green | 6 |
| Setting individual targets on the green alone | 4 |
| Putting on the green alone | 2 |
Note: SUD score of 0 = no anxiety experienced: “feeling the speed of my arms, control of my arms, and inner calmness”; SUD score of 10 = extreme anxiety: “electric shock in my arms, not in control of my arms, intense anxiety inside.”
Week 1, Session 1
The first session involved an initial formulation of the problem between the sport psychologist, EMDR therapist, and X. In this session, intervention goals were established. X stated that he wanted to be able to “go back out and play a round of golf again, just be able to hit the thing like I used too without this disease in control of me.” Further to this, he identified wanting to compete again in a local proamateur competition. An overarching goal was to recapture the level of enjoyment he used to have for golf. Once goals had been established, a graded exposure plan was constructed (see Table 1) and arrangements were made for two future sessions between the sport psychologist and X, and the EMDR therapist and X.
Week 2, Session 2
Meeting between sport psychologist and X. Following informal discussion, the sport psychologist explored X’s current state of well-being and performance. X discussed completing four practice sessions at the first two levels of exposure, with SUD scores of 8/10 and 9/10, respectively. X recognized a felt urgency to overcome the problem and reported experiencing severe anxiety just thinking about going out to practice.
Weeks 3 Through 4, Session 3
Meeting between EMDR therapist and X. After a brief review, the EMDR therapist began Phase 1 of the EMDR protocol: case formulation and client history taking (Shapiro, 1999). Having already conducted an initial formulation with the sport psychologist and X, the aim of this process was to carry out a clinical assessment and explore in more depth any underlying emotional experiences or significant events that might be associated with the performance block. During this session, X identified several significant events, including the early death of his father when he was 2 years old and adjustment to his mother’s remarriage at the age of 10. When recalling a particular period of his life involving a major career transition, he described how he “completely flipped out and just lost it.” Other life events identified included family disruption following his father’s death, the later death of his mother and sister, substantial work-related stress, and unstable relationships. More important, X highlighted substantial emotional suppression throughout his life, driven by the need to “not to be a burden to others or upset other people.” Sport-specific events identified included several performance blocks in competitive situations. The most notable of these was an experience that occurred during a team event in a professional competition when he was attempting a 3-foot putt on the 18th green, the final shot to secure the game for him and his team. This experience ultimately led to his retirement from competition a year later.
Symptoms reported at the time of these events included extreme fear, confusion, and subsequent avoidance of situations that might cause embarrassment or failure (e.g., public speaking, dancing, learning a new skill, and vomiting in public). Some of these symptoms might have been linked to an avoidance of risk and fear of failure developed in childhood: “I was over-cared for and never ever allowed to take a risk or make a mistake.” X was unable to identify a time he had failed and stated, “No. I would never attempt anything if I thought I might not be able to do it; that would just be embarrassing.”
Following the session, the EMDR therapist shared his formulation with the sport psychologist providing the following summary:
It appears to be an anxiety-based difficulty in a performance context. There are clear signs of an insecure-avoidant attachment style whereby (participant) has learnt to suppress emotion that is likely accompanied with beliefs about needing to care for others, avoid failure, and please everyone. A number of significant events have been identified that have only served to exacerbate his presentation of the problem.
This report was supported by scores revealed on the IES, for which X recorded a total score of 36 (total avoidance = 13, Mavoidance = 1.6; total intrusion = 11, Mintrusion = 1.4; total hyperarousal = 12, Mhyperarousal = 2), indicative of the extreme trauma associated with performance blocks.
Weeks 5 Through 7
During this period, X engaged in daily practice sessions using the exposure hierarchy with continued focus on the first two levels (putting on the green alone and setting individual targets on the green alone). X reported reduced SUD scores of 6/10 for both levels. X also reported that during this time, he had made several positive changes to his lifestyle (e.g., leaving the office every evening to schedule time on the putting green, time with his family, and also increased communication with close friends regarding his golf practices). Furthermore, X identified having discussed some deep felt emotion with his wife, something he had repressed to that date.
Week 8, Session 4
Session 4 comprised a review of exposure treatment between the sport psychologist and X, in which X discussed several practices completed on the first level of the hierarchy in which he experienced lower levels of anxiety (SUD = 2/10). X identified that he continued to experience increased anxiety at the second level (SUD 6/10) and so it was agreed he would continue at this level, setting individual targets for himself on the green.
Weeks 9 Through 10, Session 5
During this period, X engaged in daily practice sessions using the exposure hierarchy, initially at Levels 3 and 4; however, in the subsequent session, he reported that he had taken the opportunity to progress up to the sixth level of the hierarchy on three occasions—playing three informal friendly games. He also discussed having shared with details of the current treatment intervention with other players. X reported SUD of 9/10 and the need to return to Levels 4 and 5 (putting on the green with a professional, informal game scenario with two others) until the anxiety levels decreased.
Week 11, Session 6
Meeting between EMDR therapist and X. In accordance with Phase 2 of the EMDR protocol, the EMDR therapist explored X’s internal felt sense of safety associated with different contexts and identified a suitable internal representation of this place to return to after each reprocessing set. The therapist and X then worked together on developing an appropriate sequencing plan for the identified TMs, present triggers, and future desired outcomes identified in the formulation stage. Three memories were listed on the target-sequencing plan (SUDs respective of current anxiety felt when recalling the event):
1. 2011—Missing a 3-ft putt in a professional competition (SUD = 8/10)
2. 2006—On a training course with fellow professionals and hitting a shot on the range that skewed left. Embarrassment felt when he was asked if he wanted second attempt in front of the other professionals who were all younger than him (SUD = 9/10)
3. 2004—Missing a bunker shot in a game with the club captain (SUD = 10/10)
Processing then started on the first TM. SUD score was 8/10; negative cognitions were “I have to be perfect (and please everyone)” and “I am not in control of my own body.” Positive cognition was “I can be myself,” and the VOC was 2/7. X identified associated feelings of embarrassment and shock as well as tightness in the chest, shaky legs, and feeling hot in the face (embarrassment).
After approximately 12 sets of BLS, SUD score lowered from 8/10 to 0/10. X reported absence of tightness in the chest and stomach, reduced warmth in the face/“flush,” stillness, and mental clarity. X was unable to reactivate an image of the TM and reported “feeling nothing” when the therapist revisited this memory. The therapist observed relaxed posture and use of humor that he later described as a possible coping mechanism for underlying anxiety. The session was drawn to a close activating X’s safe place (Phase 7), after installing the positive cognition “I can be myself” with VOC of 6/7 (Phase 5), and completing a body scan (Phase 6), through which no remaining sensations were reported.
Weeks 12 Through 15, Session 7
Meeting between sport psychologist and X. Although he had not been able to practice as much as intended (causing additional frustration), X reported having taken his first few days annual leave he had ever taken and that he had played two rounds of golf: one on his own and one with two committee members, consequently progressing up toward Level 6 of the graded exposure hierarchy. X reported SUD scores of 2/10 for Level 4, 4/10 for Level 5, and 5/10 for Level 6. X agreed to continue at Level 6 for the next week, identifying a need to increase practice hours at this level. The sport psychologist explored X’s level of anxiety and experience thus far of the EMDR treatment component. X confirmed that he “felt nothing” when recalling the first TM (SUD = 0/10). However, he said that he was due to play on the same course twice in the next couple of weeks in a practice round and then again in the same event as the first TM took place. He attached a SUD score of 7/10 to this event.
Week 16, Session 8
Session 7 was held between the EMDR therapist and X and started with Phase 8 of the EMDR protocol, reevaluating the previous work. X had recalled several other memories from his past since the previous session and additional details related to events already discussed. On completing Phase 8, the therapist was concerned about remaining anxiety associated with the first TM that was readdressed with further processing. SUD score was 3/10, negative cognition was “I have to be perfect (and please everyone),” and positive cognition was “I can be myself,” with VOC 3/7. After several sets of processing, SUD score lowered to 0/10, VOC increased to 6/7. The session was concluded at this point with Phases 5–7.
Weeks 17 Through 20, Session 9
In Session 8, the sport psychologist met with X on the putting green at his club, where he continued to practice throughout the course of the conversation. X provided an update on his recent practice against the graded exposure plan, with SUD scores of 3/10 for Levels 5 and 6. X also reported that the previous day he had played a friendly round with three others at one of the courses he had experienced the problem several years ago (graded exposure Level 5). He had experienced extreme levels of anxiety from the point of leaving his house (SUD = 9/10) and that these feelings escalated throughout the day (SUD = 10/10). Physical sensations were tingling and shaking in the forearms, jerky movements on the putting green, and an “electric shock feeling” on the 18th, the same green of his initial performance block. These symptoms resulted in an inability to putt, and subsequent avoidance of finishing shots, suggesting his partner took them. This session lasted approximately 2 hours, during which X talked about the emotional, cognitive, and physical sensations associated with this experience in great depth, until he reported having more clarity and perspective toward it.
Week 21, Session 10
The session started with Phase 8 of the EMDR protocol, reviewing treatment progress. Treatment effects identified included increased communication in X’s relationships and a need to understand the context of early family bereavements. Although X wanted to contact his sister, he recognized significant avoidance with negative cognitions of “not wanting to upset her” and “not knowing how she will react.” After much discussion, X appeared to assess the situation more appropriately.
On revisiting the TM’s, three further rounds of processing were done, until X reported no further disturbance or distress, and complete absence of physical sensations including flushness, tightness, and shakiness. It was agreed that no additional processing was required for the three identified TMs but that X would consider addressing some earlier memories (e.g., death of his father and family disruption). A future template was administered at the completion of Phase 5, synthesizing X’s use of the positive cognition “I can be myself.” X agreed to continue focusing on the use of his positive cognition: “I can be myself,” protecting personal time on a daily basis and pursuing activities considered to be risky options. The sport psychologist then joined the session, and when asked to recall his first and most severe performance block experience, X reported no emotional, cognitive, or physical sensations. X identified final SUD scores of 1/10 for Level 5 of the graded exposure plan, 2/10 for Level 6, and 5/10 for Level 7. Several upcoming competitions were identified that X would enter (Level 7 of hierarchy), and he stated that he could see himself recovering fully.
Week 27, Session 11
Session 10 was conducted 5 weeks posttreatment and consisted of a full review with X, the EMDR therapist, and sport psychologist. Prior to this session, X had competed in two competitive team events (final level of graded exposure), during which he experienced mild performance-related anxiety (SUD = 4/10) but complete absence of physical sensations associated with the performance block. X confirmed that levels of anxiety and physical tension had decreased at all levels of graded exposure. The sport psychologist observed signs of physical relaxation, calmness, and improved articulation of emotion. Additional outcomes included absence of ruminative thoughts, memories, and worries associated with the identified TMs. X reported that discussing each TM and performance block openly had helped him to reappraise memories and that since doing EMDR he perceived these experiences as unimportant.
The intervention came to an end when X’s aims had been achieved. That is, he no longer suffered from the physical, emotional, or cognitive symptoms associated with the performance block, and performance had improved both in training and competition. X discussed enjoying playing again and had experienced significant improvement in social functioning.
Results
Performance Success
Prior to the start of the intervention, putting success rate was 5/10 at 3 ft and 4/10 at 4 ft distances. Postintervention these scores were 10/10 at both distances. Performance improvements were also made according to graded exposure, along which X progressed to the final level of exposure with complete absence of performance block symptoms.
Subjective Units of Distress (SUD; Wolpe, 1973)
SUD scores recorded throughout EMDR treatment demonstrated reduced anxiety levels associated with all TMs. For the first TM, SUDs reduced from 8/10 to 0/10, from 9/10 to 0/10 for the second TM, and finally from 10/10 to 0/10 for the third TM, although it should be noted that no actual processing took place for this particular TM because SUDs had reduced prior to it being targeted. This was likely a side effect of processing done on the first two TMs.
Validity of Cognition (Shapiro, 2001)
VOC scores recorded throughout EMDR treatment reflected the participants increased belief in the positive cognitions. For the first TM, these increased from 2/7 to 6/7 and from 1/7 to 7/7 for the second TM.
Impact of Event Scale (Zilberg, Weiss & Horowitz, 1982)
Prior to treatment, total score revealed on the IES was 36 (total avoidance = 13, Mavoidance = 1.6; total intrusion = 11, Mintrusion = 1.4; total hyperarousal = 12, Mhyperarousal = 2). Post intervention, this score had reduced to 0 on all aspects.
Kinematic Data
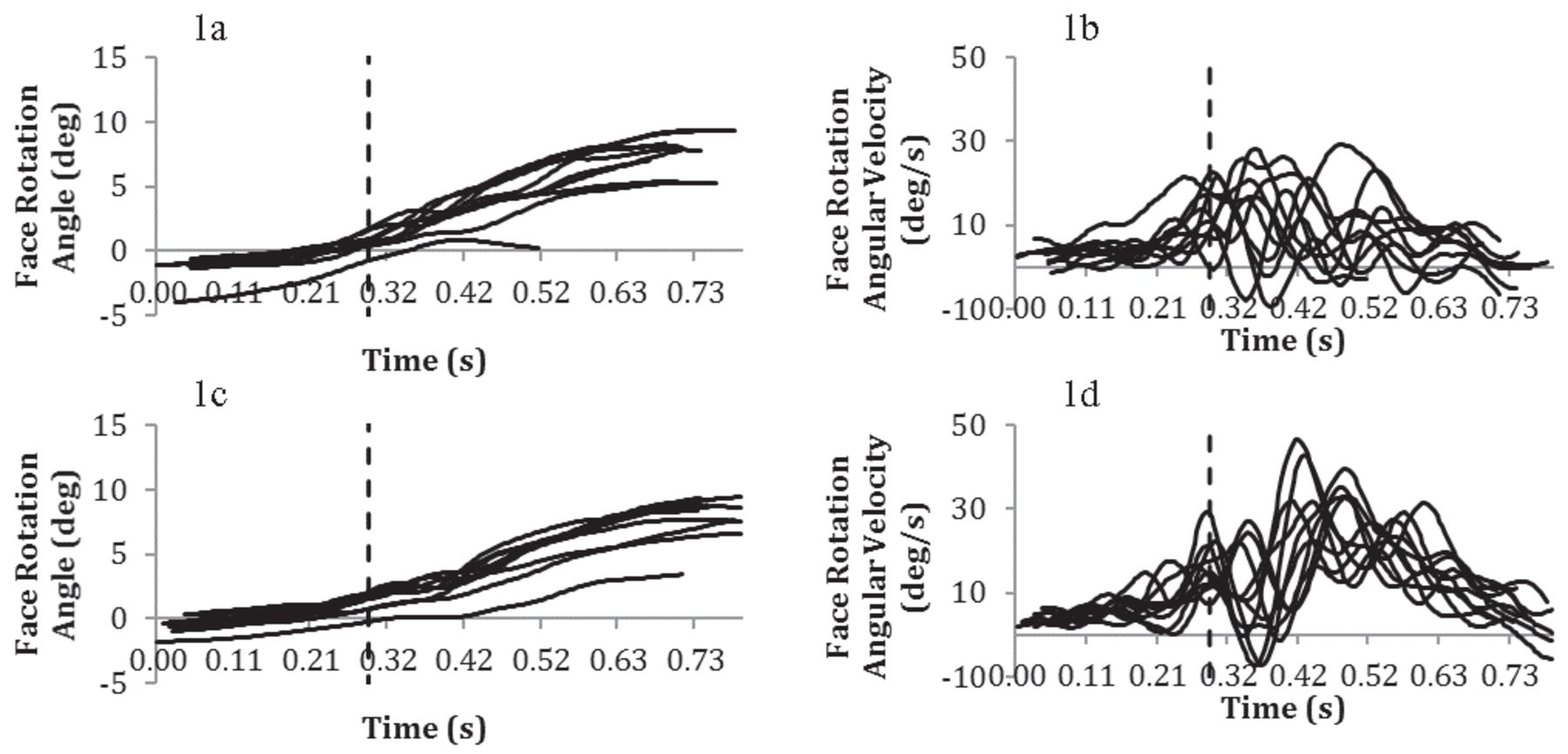
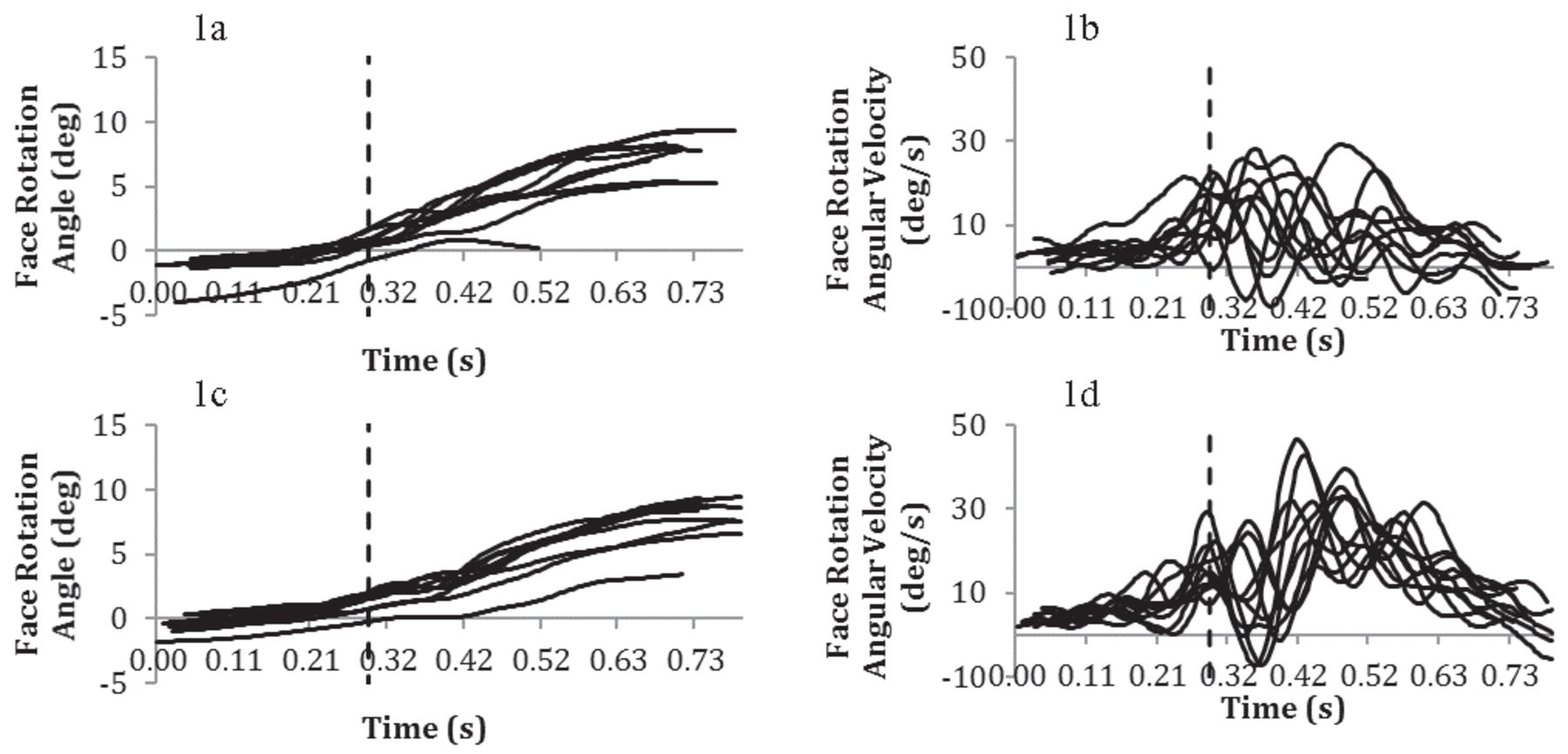
Figures 1 and 2 illustrate putter face rotation angle and putter face rotation angular velocity; from the top of the backswing through to forward swing, impact is indicated by the vertical line. Visual inspection of the data from baseline to postintervention suggests increased control over the putting stroke following treatment. More specifically, velocity of putter face rotation following treatment is illustrated by close, smooth lines that are characteristic of a smooth putting stroke, in comparison to the irregular data collected prior to treatment (Marquardt, 2009). These data suggest that the involuntary movement disturbance was causing the jerkiness of the club head on impact with the ball. This improvement also coincides with lowered levels of anxiety and increased performance success.
Preintervention data illustrating face rotation angle and face rotation angular velocity for putts from 0.91 m/3 ft (1a and 1b) and 1.22 m/4 ft (1c and 1d). Data are shown from the top of the backswing to the finish of the stroke, vertical line indicating impact.
Postintervention data illustrating face rotation angle and face rotation angular velocity for putts from 0.91 m/3 ft (2a and 2b) and 1.22 m/4 ft (2c and 2d). Data are shown from the top of the backswing to the finish of the stroke, vertical line indicating impact.

Social Validation
Following the intervention, X highlighted several improvements in performance and social functioning. For example, when asked about his level of anxiety associated with the performance block, he reported,
I can’t feel it even if I try to. I am not thinking about it at all; I don’t worry about it or get the same nerves I did because of it at all. There’s no feeling there anymore, no brake-accelerator feeling in my arms, nothing like that. I don’t think I’ll ever understand why EMDR and talking about memories has made all that freer and go away, but it has, it’s really worked. I can comprehend that it’s totally a mental thing.
The scores derived from the IES administered postintervention further support this, confirming no remaining anxiety. X indicated that he believed these improvements were a direct result of the intervention and that as a result of treatment, he was “in a better place than I have ever been before.” He talked in particular about enhanced family relations, increased communication with siblings, and an improved relationship with his wife. Improvements were also reflected in his performance on the golf course where he was no longer ruminating, losing focus, or avoiding taking putts. Interestingly, X also reported that he had stopped biting his nails, something he reported having done since childhood:
My inner thoughts weren’t even given a look in before this treatment; it was just a mess, but it’s beginning to get clearer; it’s just like little boxes opening and suddenly I am doing other things like I’ve stopped nail biting, which is completely off the wall; it was just a nervous thing that I would never have related to it but I’m beginning to understand.
X’s perception of the problem also changed:
I know if I go out there now, it’s just a completely different feeling; I feel like a different player; it [performance block] isn’t with me anymore, and I know that if I ever experienced it again that I would be able to manage my emotions way better now.
When asked about his overall performance in comparison to before the problem, he recognized that he wasn’t at the same level; however, he identified being excited to play again.
When asked to talk about the impact of the intervention on social functioning, X said, “I talk about my emotions now, and I’m not afraid to that has been such a huge turning point for me; I never spoke to anyone before.”
In a 3-month posttreatment follow-up, X reported that he was competing in professional competitions with complete absence of performance block symptoms: “I played 18 holes without a single bad feeling on the greens; it was the best I have felt for years; I have a different mindset now it’s magic!”
When reflecting on the effectiveness of EMDR, the therapist said.
The value of EMDR in this context is in its structure, specifically around creation of a safe place; it gave the physical intimacy for X to connect with and give feedback on his internal state; I think initially there was a level of embarrassment towards that but then to realize he could experience that safely was an extremely powerful part of it.
The therapist added to this that possibly, the most important aspect regarding sport was sharing the formulation of the problem with the participant and sport psychologist and educating the participant on underlying components and the impact of anxiety on the body. In terms of specific challenges for use of EMDR in elite sport, the therapist suggested,
Developing a safe therapeutic environment that is consistent is always going to be a challenge in sport, coupled with maintaining the intensity of sessions around training and competition. Also, consideration of other stakeholders (e.g., coach/performance management); they all need educating, and they all have input into the overall outcome goal.
Discussion
The emerging similarities between performance blocks and anxiety-based disorders posits that comparable treatment methods might also yield comparable outcomes. As such, this study adopted a combined intervention of EMDR therapy and graded exposure for the treatment of performance blocks in sport. Because of the lack of existing research using this method for performance blocks, this research also hoped to comprehend the participant’s experiences of receiving EMDR. It was hypothesized that by reprocessing significant life events and addressing associated psychological components, the physical symptoms of the performance block would subside. Prior to the intervention, assessment by visual observation, self-report, and performance success identified severe anxiety, involuntary movement, muscle tension, shaking, and spasms. Postintervention, these symptoms were no longer apparent. Putting success had also increased to 100% success rate at 3 and 4 ft, from 50% (3 ft) and 40% (4 ft), respectively.
Previous research using EMDR therapy has shown that an individual’s perceptions of an event and personality can alter through the course of treatment, because significant life events and associated emotions are processed (Greway, 2003). Interview data collected on completion of treatment would appear to support this, because the participant identified less importance associated with the problem, ability to articulate emotion, and considerably less rumination and obsessive behavior. Care must be taken interpreting these findings because no direct measures can be provided to support these claims. However, one direction of future enquiry would be to assess personality characteristics prior to the intervention and again on completion. Indeed, previous research has drawn links between perfectionism, rumination, reinvestment, and performance block symptoms (e.g., Bennett et al., 2016; Roberts et al., 2013). This would extend existing literature and our understanding as to whether these characteristics might be symptoms of performance blocks or individual vulnerability factors to their onset.
A central tenet of EMDR therapy is that if traumatic experiences are not processed effectively, they will become the basis of dysfunction. The participant in this study reported a history of significant life events, emotional suppression, and difficulty articulating internal experiences. During EMDR, the client is encouraged to communicate any images, thoughts, or feelings that surface, thus promoting the processing and understanding of internal experience. As identified by the participant, EMDR treatment contributed enormously to his improved understanding and articulation of emotion posttreatment. Establishing a strong therapeutic alliance between the participant, EMDR practitioner, and sport psychologist was of paramount importance in addressing these symptoms, supported by the emphasis placed on establishing psychological safety within the EMDR protocol.
The efficacy of exposure for reducing symptoms of reexperiencing, avoidance, and anxiety has received wide support, yielding the highest success rate in overcoming PTSD when compared with other forms of treatment (e.g., Taylor et al., 2003). The current findings are consistent with substantial research supporting the use of graded exposure for the reduction of avoidance and anxiety (Taylor et al., 2003). Although EMDR is favored for its lack of homework and therefore reduced treatment time (Ho & Lee, 2012), the contextual demands relating to competition calendars meant that EMDR treatment sessions were intermittently spread over the course of a relatively long period. Furthermore, multiple individuals were involved in the planning and delivery of the intervention, and therefore, additional sessions in the form of reviews and performance assessment were required. More important, findings suggest that diluted EMDR treatment with regular informal support might be as effective as more frequent sessions.
Although findings from the current case are promising, by the very nature of the study design, the results cannot be generalized to larger populations. It should be recognized that no single treatment is a panacea for every individual, and the success of the intervention might be the result of individual differences or exceptional personal histories. Furthermore, it cannot be ascertained which component of the intervention yielded most success. However, the use of objective measures, a standard EMDR treatment protocol, and social validation all assisted in increasing treatment fidelity. Furthermore, various researchers have supported the value of integrating EMDR with other treatments (e.g., Shapiro, Kaslow, & Maxfield, 2007; Shapiro, 2012). Moreover, the aim of this study was to provide an effective treatment method for performance blocks and not to directly compare the benefits of EMDR with graded exposure. It is possible that performance improved as a by-product of increasing focused practice over the course of the 27 weeks. However, the participant identified having attempted to overcome the performance block with substantial practice and technique changes over the course of several years prior to treatment with little to no success. The participant reported positive experience of talking through his emotions with both practitioners, and it is therefore likely that talk therapy contributed to improved social functioning and participant’s well-being. Establishing a strong alliance is imperative for effective treatment, enabling felt trust and safety to develop for the client. However, it is recognized that the strength of the relationship between therapist and client might determine the success of any treatment plan.
One of the potential side effects of EMDR treatment is cognitive fatigue from the increased cognitive load of processing (Shapiro, 2001). The implications of this regarding an individual’s ability to maintain physical training load in sport are huge. The current findings highlight the necessity of adopting a team approach when planning the course of treatment and that it cannot be as prescriptive as perhaps other contexts might allow. Furthermore, the motivation for using EMDR therapy in elite sport will often be driven by the need to overcome a performance problem that is disrupting an individual’s ability to compete. As such, there will be numerous stakeholders involved, all of whom should be kept informed.
Although EMDR evidently has a place in sport for the treatment of performance blocks, it would be unwise to assume the readiness of sport psychologists to deliver this treatment without appropriate clinical supervision. In many cases, it is likely that highly traumatic memories might surface, and it is imperative that the system around the individual is properly equipped to manage that. Thus, when an individual presents all of the symptoms of a performance block, it is recommended that both sport and clinical psychologists are involved in a full assessment and history taking with the athlete, following which the level of therapist experience and practitioner supervision required for treatment is carefully assessed.
In summary, this case study provides valuable insight for the use of EMDR therapy and graded exposure for the treatment of performance blocks. More specifically, it demonstrates a relationship between significant life events, anxiety, and performance blocks in sport and that addressing these components might facilitate performance improvement. The current intervention ended when the participant had achieved the goals identified from the outset: overcoming the physical symptoms associated with the performance block and therefore alleviating maladaptive cognitive, behavioral, and emotional symptoms. As a result of the intervention, the participant returned to competition with a complete absence of physical movement disruption and improved social functioning in all affected areas.
Note
- 1
To ensure anonymity, the participant in this study will be identified using the pseudonym X.
References
- E. Altenmüller, C. I. Ioannou, & A. Lee (2015). Apollo’s curse: Neurological causes of motor impairments in musicians. Progress in Brain Research, 217, 89–106. 10.1016/bs.pbr.2014.11.022
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed., pp. 5–25). Arlington, VA: Author.
- R. T. Barker, & S. B. Barker (2007). The use of EMDR in reducing presentation anxiety. Journal of EMDR Practice and Research, 1, 100–108. 10.1891/1933-3196.1.2.100
- M. A. K. Bawden, & I. W. Maynard (2001). Towards an understanding of the personal experience of the ‘yips’ in cricketers. Journal of Sports Sciences, 19, 937–953. 10.1080/026404101317108444
- J. Bennett, K. Hays, P. Lindsay, P. Olusoga, & I. W. Maynard (2015). Yips and lost move syndrome: Exploring psychological symptoms, similarities, and implications for treatment. International Journal of Sport Psychology, 46, 61–82.
- J. Bennett, M. Rotherham, K. Hays, P. Olusoga, & I. Maynard (2016). Yips and lost move syndrome: Assessing impact and exploring levels of perfectionism, rumination, and reinvestment. Sport and Exercise Psychology Review, 12.
- R. Cook-Vienot, & R. J. Taylor (2012). Comparison of eye movement desensitization and reprocessing and biofeedback/stress inoculation training in treating test anxiety. Journal of EMDR Practice and Research, 6, 62–72. 10.1891/1933-3196.6.2.62
- G. Craig (1999). Emotional freedom techniques: The manual (2nd ed.). The Sea Ranch, CA: Author.
- M. G. Craske, M. Treanor, C. C. Conway, T. Zbozinek, & B. Vervliet (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour research and therapy, 58, 10–23. 10.1016/j.brat.2014.04.006
- E. Dautovic, C. de Roos, Y. van Rood, A. Dommerholt, & R. Rodenburg (2016). Pediatric seizure-related posttraumatic stress and anxiety symptoms treated with EMDR: A case series. European Journal of Psychotraumatology, 7, 30123. 10.3402/ejpt.v7.30123
- M. C. Day, J. Thatcher, I. Greenless, & B. Woods (2006). The causes of and psychological responses to lost movement syndrome in national level trampolinists. Journal of Applied Sport Psychology, 18, 151–166. 10.1080/10413200600653782
- P. Gauvreau, & S. Bouchard (2008). Preliminary evidence for the efficacy of EMDR in treating generalized anxiety disorder. Journal of EMDR Practice and Research, 2, 26–40. 10.1891/1933-3196.2.1.26
- G. S. Greway (2003). Personality change in trauma victims by the use of eye movement desensitization and reprocessing, resource development and installation, and emotional freedom techniques. Dissertation Abstracts International: Section B. Sciences and Engineering, 64(4-B), 1902.
- E. Grey (2011). A pilot study of concentrated EMDR: A brief report. Journal of EMDR Practice and Research, 5, 14–24. 10.1891/1933-3196.5.1.14
- M. S. K. Ho, & C. W. Lee (2012). Cognitive behavior therapy versus eye movement desensitization and reprocessing for post-traumatic disorder: Is it all in the homework then? European Review of Applied Psychology, 62, 253–260. 10.1016/j.erap.2012.08.001
- M. Kindt (2014). A behavioural neuroscience perspective on the aetiology and treatment of anxiety disorders. Behaviour research and therapy, 62, 24–36. 10.1016/j.brat.2014.08.012
- M. Klämpfl, B. Lobinger, & M. Raab (2013). How to detect the yips in golf. Human Movement Science, 32, 1270–1287. 10.1016/j.humov.2013.04.004
- J. LeDoux (2014). Coming to terms with fear. Proceedings of the National Academy of Sciences of the United States of America, 111, 2871–2878. 10.1073/pnas.1400335111
- J. Lendl, & S. Foster (1997). EMDR performance enhancement for the workplace: A practitioners’ manual. San Jose, CA: Performance Enhancement Unlimited.
- P. A. Levine (1997). Waking the tiger: Healing trauma: The innate capacity to transform overwhelming experiences. Berkeley, CA: North Atlantic Books.
- H. J. Lipke, & A. Botkin (1993). Case studies of eye movement desensitization and reprocessing (EMDR) with chronic post-traumatic stress disorder. Psychotherapy, 29, 591–595.
- R. H. Logie (2014). Visuo-spatial working memory. Hove, United Kingdom: Psychology Press.
- C. Marquardt (2009). The vicious circle involved in the development of the yips. International Journal of Sports Science and Coaching, 4(Suppl. 1), 67–88. 10.1260/174795409789577506
- J. Marr (2012). EMDR treatment of obsessive-compulsive disorder: Preliminary research. Journal of EMDR Research and Practice, 6, 2–15. 10.1891/1933-3196.6.1.2
- L. Maxfield, & W. T. Melnyk (2000). Single session treatment of test anxiety with eye movement desensitization and reprocessing (EMDR). International Journal of Stress Management, 7, 87–101. 10.1023/A:1009580101287
- National Institute for Health and Care Excellence. (2005). Guidelines for posttraumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care. Retrieved from http://www.nice.org.uk
- N. P. Novo Navarro, R. Landin-Romero, R. Guardiola-Wanden-Berghe, A. Moreno-Alcázar, A. Valiente-Gómez, W. Lupo, . . . B. L. Amann (2016). 25 Years of eye movement desensitization and reprocessing (EMDR): The EMDR therapy protocol, hypotheses of its mechanism of action and a systematic review of its efficacy in the treatment of post-traumatic stress disorder. Revista de Psiquiatria y Salud Mental. 10.1016/j.rpsm.2015.12.002
- U. Oren, & R. Solomon (2012). EMDR therapy: An overview of its development and mechanisms of action. European Review of Applied Psychology, 62, 197–203. 10.1016/j.erap.2012.08.005
- M. Q. Patton (2002). Qualitative research & evaluation methods (3rd ed.). Thousand Oaks, CA: Sage.
- P. B. Philippen, A. Legler, W. M. Land, C. Schuetz, & T. Schack (2014). Diagnosing and measuring the yips in golf putting: A kinematic description of the involuntary movement component that is the yips. Sport, Exercise, and Performance Psychology, 3, 149–162. 10.1037/spy0000020
- R. J. Ricci, C. A. Clayton, S. Foster, I. Jarero, B. Litt, L. Artigas, & S. Kamin (2009). Special applications of EMDR: Treatment of performance anxiety, sex offenders, couples, families, and traumatized groups. Journal of EMDR Practice and Research, 3, 279–288. 10.1891/1933-3196.3.4.279
- R. Roberts, M. Rotheram, I. Maynard, O. Thomas, & T. Woodman (2013). Perfectionism and the ‘yips’: An initial investigation. The Sport Psychologist, 27, 53–61.
- M. Rotheram, I. W. Maynard, O. Thomas, M. Bawden, & L. Francis (2012). Preliminary evidence for the treatment of type I ‘yips’: The efficacy of the emotional freedom techniques. The Sport Psychologist, 26, 551–570.
- M. Rotheram, O. Thomas, M. Bawden, & I. Maynard (2007). Understanding the ‘yips’ in sport: A grounded theory interview study. Journal of Sports Sciences, 25, 323–324.
- M. C. Russell (2006). Treating combat-related stress disorders: A multiple case study utilizing eye movement desensitization and reprocessing (EMDR) with battlefield casualties from the Iraqi war. Military Psychology, 18, 1–18.
- R. Scaer (2014). The body bears the burden: Trauma, dissociation, and disease (3rd ed.). New York, NY: Routledge.
- F. Shapiro (1999). Eye movement desensitization and reprocessing (EMDR) and the anxiety disorders: Clinical and research implications of an integrated psychotherapy treatment. Journal of Anxiety Disorders, 13, 35–67. 10.1016/S0887-6185(98)00038-3
- F. Shapiro (2001). Eye movement desensitization and reprocessing (2nd ed.). New York, NY: Guildford Press.
- F. Shapiro (2007). EMDR, adaptive information processing, and case conceptualization. Journal of EMDR Practice and Research, 1, 68–87. 10.1891/1933-3196.1.2.68
- F. Shapiro (2012). EMDR therapy: An overview of current and future research. European Review of Applied Psychology, 62, 193–195. 10.1016/j.erap.2012.09.005
- F. Shapiro, F. W. Kaslow, & L. Maxfield (2007). Handbook of EMDR and family therapy processes. Hoboken, NJ: John Wiley & Sons.
- E. C. Sundin, & M. J. Horowitz (2002). Impact of Event Scale: Psychometric properties. British Journal of Psychiatry, 180, 205–209.
- S. Taylor, D. S. Thordarson, L. Maxfield, I. C. Fedoroff, K. Lovell, & J. Ogrodniczuk (2003). Comparative efficacy, speed, and adverse effects of three PTSD treatments: Exposure therapy, EMDR, and relaxation training. Journal of Consulting and Clinical Psychology, 71, 330–338. 10.1037/0022-006X.71.1.330
- M. Thomas, K. D. Vuong, & J. Jankovic (2006). Long-term prognosis of patients with psychogenic movement disorders. Parkinsonism & Related Disorders, 12, 382–387. 10.1016/j.parkreldis.2006.03.005
- J. Wolpe (1973). The practice of behavior therapy. New York, NY: Pergamon.
- J. Wolpe (1982). The practice of behavior therapy (3rd ed.). New York, NY: Pergamon Press.
- World Health Organization. (2013). Guidelines specifically developed for the management of conditions specifically related to stress. Geneva, Switzerland: Author.
- N. J. Zilberg, D. S. Weiss, & M. J. Horowitz (1982). Impact of event scale: A cross-validation study and some empirical evidence supporting a conceptual model of stress response syndromes. Journal of Consulting and Clinical Psychology, 50, 407–414. 10.1037/0022-006X.50.3.407
Figures
Preintervention data illustrating face rotation angle and face rotation angular velocity for putts from 0.91 m/3 ft (1a and 1b) and 1.22 m/4 ft (1c and 1d). Data are shown from the top of the backswing to the finish of the stroke, vertical line indicating impact.
 View in Context
View in ContextPostintervention data illustrating face rotation angle and face rotation angular velocity for putts from 0.91 m/3 ft (2a and 2b) and 1.22 m/4 ft (2c and 2d). Data are shown from the top of the backswing to the finish of the stroke, vertical line indicating impact.
 View in Context
View in ContextTables
| Step | SUD Score (0–10) |
|---|---|
| Playing an individual event and entering a scorecard | 10 |
| Playing a round as part of a team | 9 |
| Game scenario with two other players | 8 |
| Putting with another pro on the green | 7 |
| Putting with another player on the green | 6 |
| Setting individual targets on the green alone | 4 |
| Putting on the green alone | 2 |
Note: SUD score of 0 = no anxiety experienced: “feeling the speed of my arms, control of my arms, and inner calmness”; SUD score of 10 = extreme anxiety: “electric shock in my arms, not in control of my arms, intense anxiety inside.”
| Period | Abstract | Full | Total | |
|---|---|---|---|---|
| Apr 2024 | 23 | 18 | 11 | 52 |
| Mar 2024 | 24 | 14 | 8 | 46 |
| Feb 2024 | 42 | 24 | 11 | 77 |
| Jan 2024 | 56 | 10 | 5 | 71 |
| Dec 2023 | 52 | 13 | 12 | 77 |
| Nov 2023 | 34 | 22 | 6 | 62 |
| Oct 2023 | 26 | 18 | 2 | 46 |
| Sep 2023 | 45 | 8 | 13 | 66 |
| Aug 2023 | 20 | 14 | 8 | 42 |
| Jul 2023 | 37 | 17 | 3 | 57 |
| Jun 2023 | 22 | 21 | 8 | 51 |
| May 2023 | 45 | 19 | 12 | 76 |
| Apr 2023 | 35 | 67 | 8 | 110 |
| Mar 2023 | 29 | 26 | 13 | 68 |
| Feb 2023 | 35 | 329 | 6 | 370 |
| Jan 2023 | 27 | 33 | 23 | 83 |
| Dec 2022 | 22 | 25 | 11 | 58 |
| Nov 2022 | 34 | 42 | 18 | 94 |
| Oct 2022 | 35 | 26 | 18 | 79 |
| Sep 2022 | 28 | 12 | 10 | 50 |
| Aug 2022 | 9 | 12 | 4 | 25 |
| Jul 2022 | 18 | 16 | 9 | 43 |
| Jun 2022 | 26 | 16 | 6 | 48 |
| May 2022 | 26 | 20 | 8 | 54 |
| Apr 2022 | 41 | 20 | 13 | 74 |
| Mar 2022 | 42 | 30 | 15 | 87 |
| Feb 2022 | 22 | 25 | 10 | 57 |
| Jan 2022 | 18 | 28 | 6 | 52 |
| Dec 2021 | 16 | 23 | 9 | 48 |
| Nov 2021 | 34 | 24 | 11 | 69 |
| Oct 2021 | 26 | 25 | 4 | 55 |
| Sep 2021 | 19 | 27 | 6 | 52 |
| Aug 2021 | 10 | 22 | 13 | 45 |
| Jul 2021 | 18 | 22 | 7 | 47 |
| Jun 2021 | 15 | 7 | 4 | 26 |
| May 2021 | 18 | 20 | 7 | 45 |
| Apr 2021 | 19 | 16 | 3 | 38 |
| Mar 2021 | 44 | 19 | 6 | 69 |
| Feb 2021 | 41 | 14 | 1 | 56 |
| Jan 2021 | 225 | 19 | 4 | 248 |
| Dec 2020 | 52 | 24 | 6 | 82 |
| Nov 2020 | 9 | 22 | 5 | 36 |
| Oct 2020 | 20 | 30 | 5 | 55 |
| Sep 2020 | 17 | 16 | 1 | 34 |
| Aug 2020 | 21 | 11 | 3 | 35 |
| Jul 2020 | 9 | 15 | 0 | 24 |
| Jun 2020 | 17 | 13 | 2 | 32 |
| May 2020 | 19 | 38 | 2 | 59 |
| Apr 2020 | 48 | 16 | 8 | 72 |
| Mar 2020 | 96 | 33 | 7 | 136 |
| Feb 2020 | 95 | 9 | 1 | 105 |
| Jan 2020 | 78 | 20 | 13 | 111 |
| Dec 2019 | 84 | 9 | 2 | 95 |
| Nov 2019 | 19 | 11 | 1 | 31 |
| Oct 2019 | 9 | 11 | 2 | 22 |
| Sep 2019 | 2 | 2 | 2 | 6 |
| Aug 2019 | 2 | 4 | 1 | 7 |
| Jul 2019 | 4 | 12 | 2 | 18 |
| Jun 2019 | 12 | 4 | 3 | 19 |
| May 2019 | 13 | 10 | 6 | 29 |
| Apr 2019 | 3 | 17 | 5 | 25 |
| Mar 2019 | 2 | 14 | 109 | 125 |
| Feb 2019 | 10 | 9 | 4 | 23 |
| Jan 2019 | 9 | 2 | 3 | 14 |
| Dec 2018 | 12 | 2 | 0 | 14 |
| Nov 2018 | 5 | 0 | 0 | 5 |
| Oct 2018 | 19 | 1 | 2 | 22 |
| Sep 2018 | 7 | 0 | 1 | 8 |
| Aug 2018 | 6 | 1 | 3 | 10 |
| Jul 2018 | 8 | 0 | 2 | 10 |
| Jun 2018 | 2 | 1 | 1 | 4 |
| May 2018 | 0 | 0 | 1 | 1 |
